Exhibit 99.02
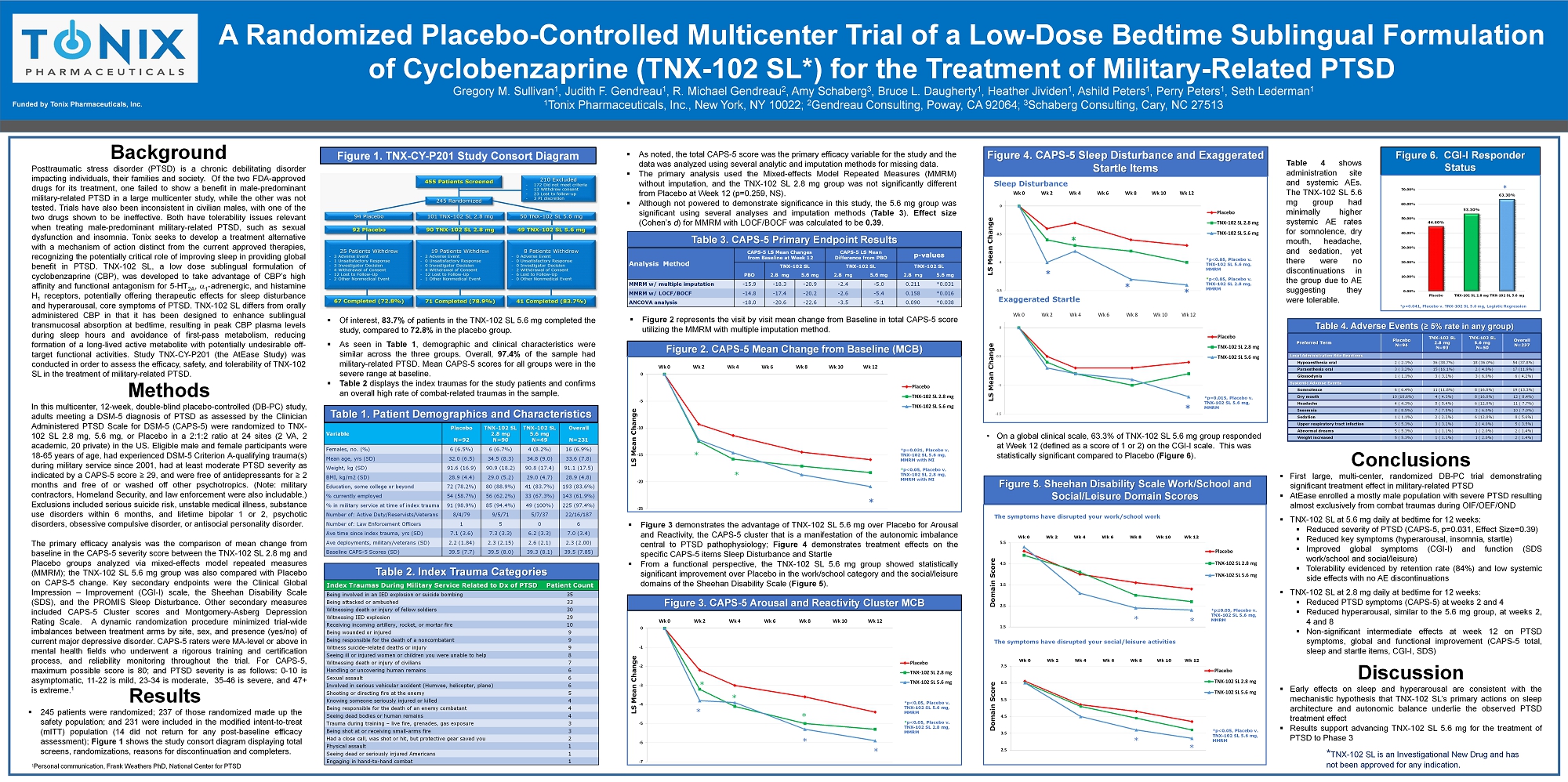
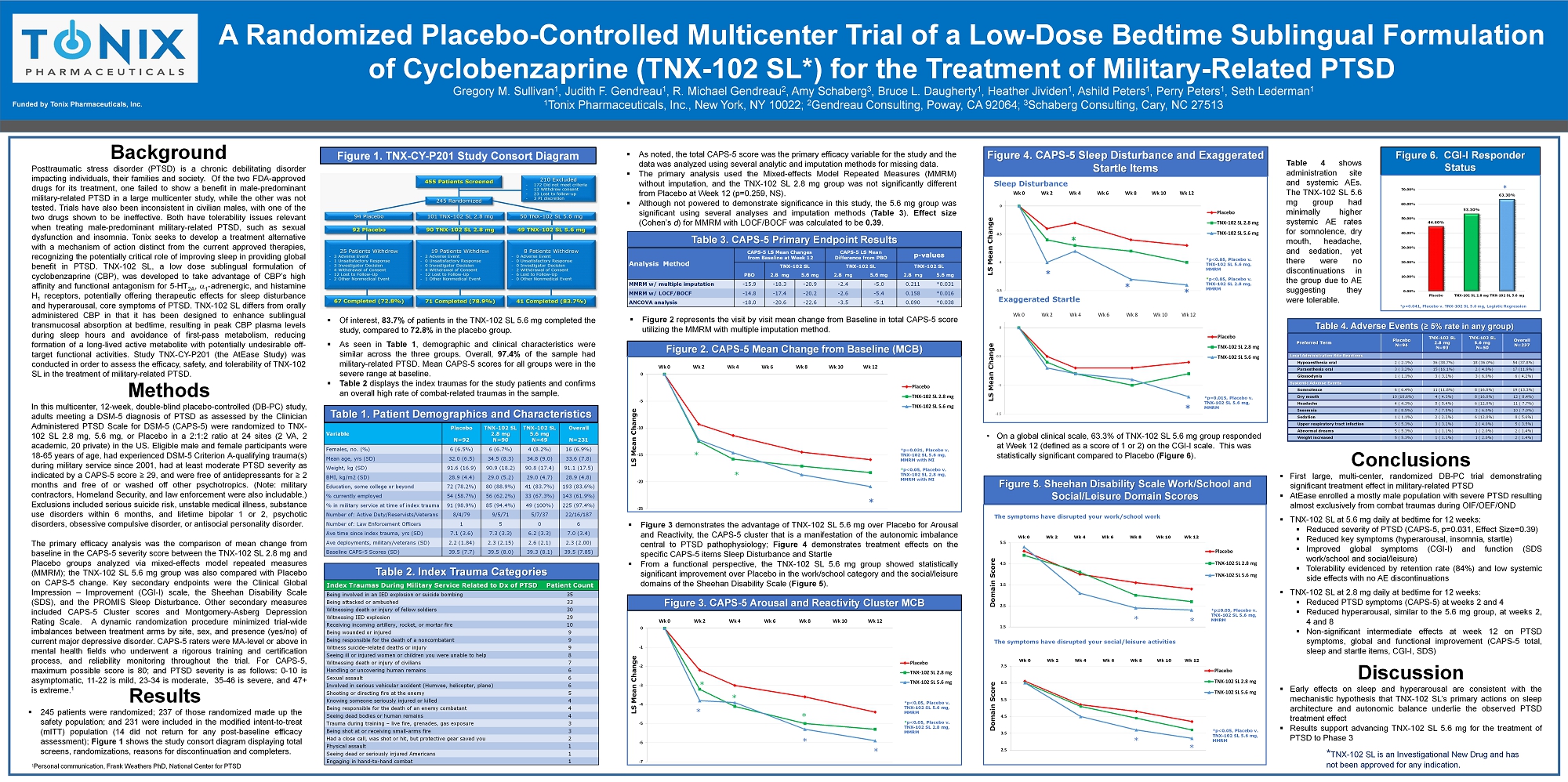
Background Posttraumatic stress disorder (PTSD) is a chronic debilitating disorder impacting individuals, their families and society . Of the two FDA - approved drugs for its treatment, one failed to show a benefit in male - predominant military - related PTSD in a large multicenter study, while the other was not tested . Trials have also been inconsistent in civilian males, with one of the two drugs shown to be ineffective . Both have tolerability issues relevant when treating male - predominant military - related PTSD, such as sexual dysfunction and insomnia . Tonix seeks to develop a treatment alternative with a mechanism of action distinct from the current approved therapies, recognizing the potentially critical role of improving sleep in providing global benefit in PTSD . TNX - 102 SL, a low dose sublingual formulation of cyclobenzaprine (CBP), was developed to take advantage of CBP’s high affinity and functional antagonism for 5 - HT 2 A , a 1 - adrenergic, and histamine H 1 receptors, potentially offering therapeutic effects for sleep disturbance and hyperarousal, core symptoms of PTSD . TNX - 102 SL differs from orally administered CBP in that it has been designed to enhance sublingual transmucosal absorption at bedtime, resulting in peak CBP plasma levels during sleep hours and avoidance of first - pass metabolism, reducing formation of a long - lived active metabolite with potentially undesirable off - target functional activities . Study TNX - CY - P 201 (the AtEase Study) was conducted in order to assess the efficacy, safety, and tolerability of TNX - 102 SL in the treatment of military - related PTSD . Gregory M. Sullivan 1 , Judith F. Gendreau 1 , R. Michael Gendreau 2 , Amy Schaberg 3 , Bruce L. Daugherty 1 , Heather Jividen 1 , Ashild Peters 1 , Perry Peters 1 , Seth Lederman 1 1 Tonix Pharmaceuticals, Inc., New York, NY 10022; 2 Gendreau Consulting, Poway, CA 92064; 3 Schaberg Consulting, Cary, NC 27513 A Randomized Placebo - Controlled Multicenter Trial of a Low - Dose Bedtime Sublingual Formulation of Cyclobenzaprine (TNX - 102 SL*) for the Treatment of Military - Related PTSD Funded by Tonix Pharmaceuticals, Inc. 34% 9.8% Conclusions ▪ First large, multi - center, randomized DB - PC trial demonstrating significant treatment effect in military - related PTSD ▪ AtEase enrolled a mostly male population with severe PTSD resulting almost exclusively from combat traumas during OIF/OEF/OND ▪ TNX - 102 SL at 5 . 6 mg daily at bedtime for 12 weeks : ▪ Reduced severity of PTSD (CAPS - 5 , p= 0 . 031 , Effect Size= 0 . 39 ) ▪ Reduced key symptoms (hyperarousal, insomnia, startle) ▪ Improved global symptoms (CGI - I) and function (SDS work/school and social/leisure) ▪ Tolerability evidenced by retention rate ( 84 % ) and low systemic side effects with no AE discontinuations ▪ TNX - 102 SL at 2 . 8 mg daily at bedtime for 12 weeks : ▪ Reduced PTSD symptoms (CAPS - 5 ) at weeks 2 and 4 ▪ Reduced hyperarousal, similar to the 5 . 6 mg group, at weeks 2 , 4 and 8 ▪ Non - significant intermediate effects at week 12 on PTSD symptoms, global and functional improvement (CAPS - 5 total, sleep and startle items, CGI - I, SDS) Discussion ▪ Early effects on sleep and hyperarousal are consistent with the mechanistic hypothesis that TNX - 102 SL’s primary actions on sleep architecture and autonomic balance underlie the observed PTSD treatment effect ▪ Results support advancing TNX - 102 SL 5 . 6 mg for the treatment of PTSD to Phase 3 * TNX - 102 SL is an Investigational New Drug and has not been approved for any indication. Methods In this multicenter, 12 - week, double - blind placebo - controlled (DB - PC) study, adults meeting a DSM - 5 diagnosis of PTSD as assessed by the Clinician Administered PTSD Scale for DSM - 5 (CAPS - 5 ) were randomized to TNX - 102 SL 2 . 8 mg, 5 . 6 mg, or Placebo in a 2 : 1 : 2 ratio at 24 sites ( 2 VA, 2 academic, 20 private) in the US . Eligible male and female participants were 18 - 65 years of age, had experienced DSM - 5 Criterion A - qualifying trauma(s) during military service since 2001 , had at least moderate PTSD severity as indicated by a CAPS - 5 score ≥ 29 , and were free of antidepressants for ≥ 2 months and free of or washed off other psychotropics . (Note : military contractors, Homeland Security, and law enforcement were also includable . ) Exclusions included serious suicide risk, unstable medical illness, substance use disorders within 6 months, and lifetime bipolar 1 or 2 , psychotic disorders, obsessive compulsive disorder, or antisocial personality disorder . The primary efficacy analysis was the comparison of mean change from baseline in the CAPS - 5 severity score between the TNX - 102 SL 2 . 8 mg and Placebo groups analyzed via mixed - effects model repeated measures (MMRM) ; the TNX - 102 SL 5 . 6 mg group was also compared with Placebo on CAPS - 5 change . Key secondary endpoints were the Clinical Global Impression – Improvement (CGI - I) scale, the Sheehan Disability Scale (SDS), and the PROMIS Sleep Disturbance . Other secondary measures included CAPS - 5 Cluster scores and Montgomery - Asberg Depression Rating Scale . A dynamic randomization procedure minimized trial - wide imbalances between treatment arms by site, sex, and presence (yes/no) of current major depressive disorder . CAPS - 5 raters were MA - level or above in mental health fields who underwent a rigorous training and certification process, and reliability monitoring throughout the trial . For CAPS - 5 , maximum possible score is 80 ; and PTSD severity is as follows : 0 - 10 is asymptomatic, 11 - 22 is mild, 23 - 34 is moderate, 35 - 46 is severe, and 47 + is extreme . 1 Figure 2. CAPS - 5 Mean Change from Baseline (MCB) Table 1. Patient Demographics and Characteristics Figure 6. CGI - I Responder Status Preferred Term Placebo N=94 TNX - 102 SL 2.8 mg N=93 TNX - 102 SL 5.6 mg N=50 Overall N=237 Local Administration Site Reactions Hypoaesthesia oral 2 ( 2.1%) 36 (38.7%) 18 (36.0%) 54 (37.8%) Paraesthesia oral 3 ( 3.2%) 15 (16.1%) 2 ( 4.0%) 17 (11.9%) Glossodynia 1 ( 1.1%) 3 ( 3.2%) 3 ( 6.0%) 6 ( 4.2%) Systemic Adverse Events Somnolence 6 ( 6.4%) 11 (11.8%) 8 (16.0%) 19 (13.3%) Dry mouth 10 (10.6%) 4 ( 4.3%) 8 (16.0%) 12 ( 8.4%) Headache 4 ( 4.3%) 5 ( 5.4%) 6 (12.0%) 11 ( 7.7%) Insomnia 8 ( 8.5%) 7 ( 7.5%) 3 ( 6.0%) 10 ( 7.0%) Sedation 1 ( 1.1%) 2 ( 2.2%) 6 (12.0%) 8 ( 5.6%) Upper respiratory tract infection 5 ( 5.3%) 3 ( 3.2%) 2 ( 4.0%) 5 ( 3.5%) Abnormal dreams 5 ( 5.3%) 1 ( 1.1%) 1 ( 2.0%) 2 ( 1.4%) Weight increased 5 ( 5.3%) 1 ( 1.1%) 1 ( 2.0%) 2 ( 1.4%) Table 4. Adverse Events (≥ 5% rate in any group) Figure 5. Sheehan Disability Scale Work/School and Social/Leisure Domain Scores -25 -20 -15 -10 -5 0 Wk 0 Wk 2 Wk 4 Wk 6 Wk 8 Wk 10 Wk 12 Placebo TNX-102 SL 2.8 mg TNX-102 SL 5.6 mg * Variable Placebo N=92 TNX - 102 SL 2.8 mg N=90 TNX - 102 SL 5.6 mg N=49 Overall N=231 Females, no. (%) 6 (6.5%) 6 (6.7%) 4 (8.2%) 16 (6.9%) Mean age, yrs (SD) 32.0 (6.5) 34.5 (8.3) 34.8 (9.0) 33.6 (7.8) Weight, kg (SD) 91.6 (16.9) 90.9 (18.2) 90.8 (17.4) 91.1 (17.5) BMI, kg/m2 (SD) 28.9 (4.4) 29.0 (5.2) 29.0 (4.7) 28.9 (4.8) Education, some college or beyond 72 (78.2%) 80 (88.9%) 41 (83.7%) 193 (83.6%) % currently employed 54 (58.7%) 56 (62.2%) 33 (67.3%) 143 (61.9%) % in military service at time of index trauma 91 (98.9%) 85 (94.4%) 49 (100%) 225 (97.4%) Number of: A ctive Duty /R eservists/Veterans 8/4/79 9/5/71 5/7/37 22/16/187 Number of: Law Enforcement Officers 1 5 0 6 Ave time since index trauma, yrs (SD) 7.1 (3.6) 7.3 (3.3) 6.2 (3.3) 7.0 (3.4) Ave deployments, military /veterans (SD) 2.2 (1.84) 2.3 (2.15) 2.6 (2.1) 2.3 (2.00) Baseline CAPS - 5 Scores (SD) 39.5 (7.7) 39.5 (8.0) 39.3 (8.1) 39.5 (7.85) -7 -6 -5 -4 -3 -2 -1 0 Wk 0 Wk 2 Wk 4 Wk 6 Wk 8 Wk 10 Wk 12 Placebo TNX-102 SL 2.8 mg TNX-102 SL 5.6 mg * * * Figure 3. CAPS - 5 Arousal and Reactivity Cluster MCB * * p=0.031, Placebo v. TNX - 102 SL 5.6 mg, MMRM with MI * p<0.05, P lacebo v. TNX - 102 SL 2.8 mg, MMRM with MI * * * *p<0.05, Placebo v. TNX - 102 SL 5.6 mg, MMRM * p<0.05, Placebo v. TNX - 102 SL 2.8 mg, MMRM 44.60% 53.30% 63.30% 0.00% 10.00% 20.00% 30.00% 40.00% 50.00% 60.00% 70.00% Placebo TNX-102 SL 2.8 mg TNX-102 SL 5.6 mg * 1.5 2.5 3.5 4.5 5.5 Wk 0 Wk 2 Wk 4 Wk 6 Wk 8 Wk 10 Wk 12 Placebo TNX-102 SL 2.8 mg TNX-102 SL 5.6 mg 2.5 3.5 4.5 5.5 6.5 7.5 Wk 0 Wk 2 Wk 4 Wk 6 Wk 8 Wk 10 Wk 12 Placebo TNX-102 SL 2.8 mg TNX-102 SL 5.6 mg The symptoms have disrupted your work/school work * * * * The symptoms have disrupted your social/leisure activities *p ≤ 0.05, Placebo v. TNX - 102 SL 5.6 mg, MMRM *p<0.05, Placebo v. TNX - 102 SL 5.6 mg, MMRM Figure 4. CAPS - 5 Sleep Disturbance and Exaggerated Startle Items -1.5 -1 -0.5 0 Wk 0 Wk 2 Wk 4 Wk 6 Wk 8 Wk 10 Wk 12 Placebo TNX-102 SL 2.8 mg TNX-102 SL 5.6 mg -1.5 -1 -0.5 0 Wk 0 Wk 2 Wk 4 Wk 6 Wk 8 Wk 10 Wk 12 Placebo TNX-102 SL 2.8 mg TNX-102 SL 5.6 mg Sleep Disturbance Exaggerated Startle * * * * * * p=0.015, Placebo v. TNX - 102 SL 5.6 mg, MMRM *p<0.05, Placebo v. TNX - 102 SL 5.6 mg, MMRM * p<0.05, Placebo v. TNX - 102 SL 2.8 mg, MMRM Figure 1. TNX - CY - P201 Study Consort Diagram Results ▪ 245 patients were randomized ; 237 of those randomized made up the safety population ; and 231 were included in the modified intent - to - treat ( mITT ) population ( 14 did not return for any post - baseline efficacy assessment) ; Figure 1 shows the study consort diagram displaying total screens , randomizations, reasons for discontinuation and completers . Analysis Method CAPS - 5 LS Mean Changes from Baseline at Week 12 CAPS - 5 LS Mean Difference from PBO p - values TNX - 102 SL TNX - 102 SL TNX - 102 SL PBO 2.8 mg 5.6 mg 2.8 mg 5.6 mg 2.8 mg 5.6 mg MMRM w/ multiple imputation - 15.9 - 18.3 - 20.9 - 2.4 - 5.0 0.211 *0.031 MMRM w/ LOCF/BOCF - 14.8 - 17.4 - 20.2 - 2.6 - 5.4 0.158 *0.016 ANCOVA analysis - 18.0 - 20.6 - 22.6 - 3.5 - 5.1 0.090 *0.038 Table 3. CAPS - 5 Primary Endpoint Results ▪ Of interest, 83 . 7 % of patients in the TNX - 102 SL 5 . 6 mg completed the study, compared to 72 . 8 % in the placebo group . ▪ As seen in Table 1 , demographic and clinical characteristics were similar across the three groups . Overall, 97 . 4 % of the sample had military - related PTSD . Mean CAPS - 5 scores for all groups were in the severe range at baseline . ▪ Table 2 displays the index traumas for the study patients and confirms an overall high rate of combat - related traumas in the sample . * Index Traumas During Military Service Related to Dx of PTSD Patient Count Being involved in an IED explosion or suicide bombing 35 Being attacked or ambushed 33 Witnessing death or injury of fellow soldiers 30 Witnessing IED explosion 29 Receiving incoming artillery, rocket, or mortar fire 10 Being wounded or injured 9 Being responsible for the death of a noncombatant 9 Witness suicide - related deaths or injury 9 Seeing ill or injured women or children you were unable to help 8 Witnessing death or injury of civilians 7 Handling or uncovering human remains 6 Sexual assault 6 Involved in serious vehicular accident (Humvee, helicopter, plane) 6 Shooting or directing fire at the enemy 5 Knowing someone seriously injured or killed 4 Being responsible for the death of an enemy combatant 4 Seeing dead bodies or human remains 4 T rauma during training – live fire, grenades, gas exposure 3 Being shot at or receiving small - arms fire 3 Had a close call, was shot or hit, but protective gear saved you 2 Physical assault 1 Seeing dead or seriously injured Americans 1 Engaging in hand - to - hand combat 1 Table 2. Index Trauma Categories ▪ As noted, the total CAPS - 5 score was the primary efficacy variable for the study and the data was analyzed using several analytic and imputation methods for missing data . ▪ The primary analysis used the Mixed - effects Model Repeated Measures (MMRM) without imputation, and the TNX - 102 SL 2 . 8 mg group was not significantly different from Placebo at Week 12 (p= 0 . 259 , NS) . ▪ Although not powered to demonstrate significance in this study, the 5 . 6 mg group was significant using several analyses and imputation methods ( Table 3 ) . Effect size (Cohen’s d ) for MMRM with LOCF/BOCF was calculated to be 0 . 39 . ▪ Figure 2 represents the visit by visit mean change from Baseline in total CAPS - 5 score utilizing the MMRM with multiple imputation method . ▪ Figure 3 demonstrates the advantage of TNX - 102 SL 5 . 6 mg over P lacebo for Arousal and Reactivity, the CAPS - 5 cluster that is a manifestation of the autonomic imbalance central to PTSD pathophysiology ; Figure 4 demonstrates treatment effects on the specific CAPS - 5 items Sleep Disturbance and Startle ▪ From a functional perspective, the TNX - 102 SL 5 . 6 mg group showed statistically significant improvement over Placebo in the work/school category and the social/leisure domains of the Sheehan Disability Scale ( Figure 5 ) . Table 4 shows administration site and systemic AEs . The TNX - 102 SL 5 . 6 mg group had minimally higher systemic AE rates for somnolence, dry mouth, headache, and sedation, yet there were no discontinuations in the group due to AE suggesting they were tolerable . 1 P ersonal communication, Frank Weathers PhD, National Center for PTSD * p=0.041, Placebo v. TNX - 102 SL 5.6 mg, Logistic Regression • On a global clinical scale, 63.3% of TNX - 102 SL 5.6 mg group responded at Week 12 (defined as a score of 1 or 2) on the CGI - I scale. This was statistically significant compared to Placebo ( Figure 6 ). LS Mean Change LS Mean Change LS Mean Change LS Mean Change Domain Score Domain Score