Tonix Pharmaceuticals Holding Corp. 8-K
Exhibit 99-03
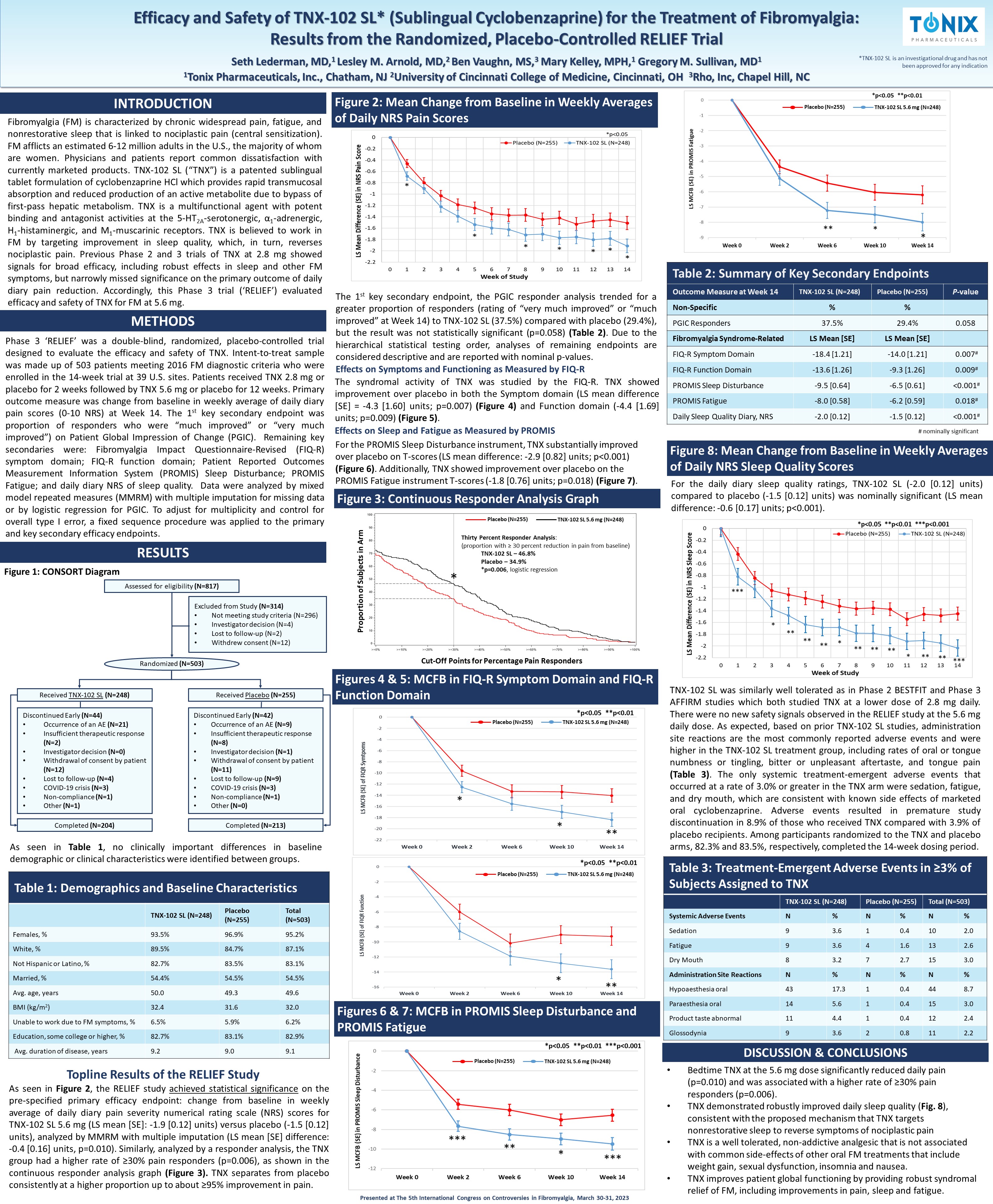
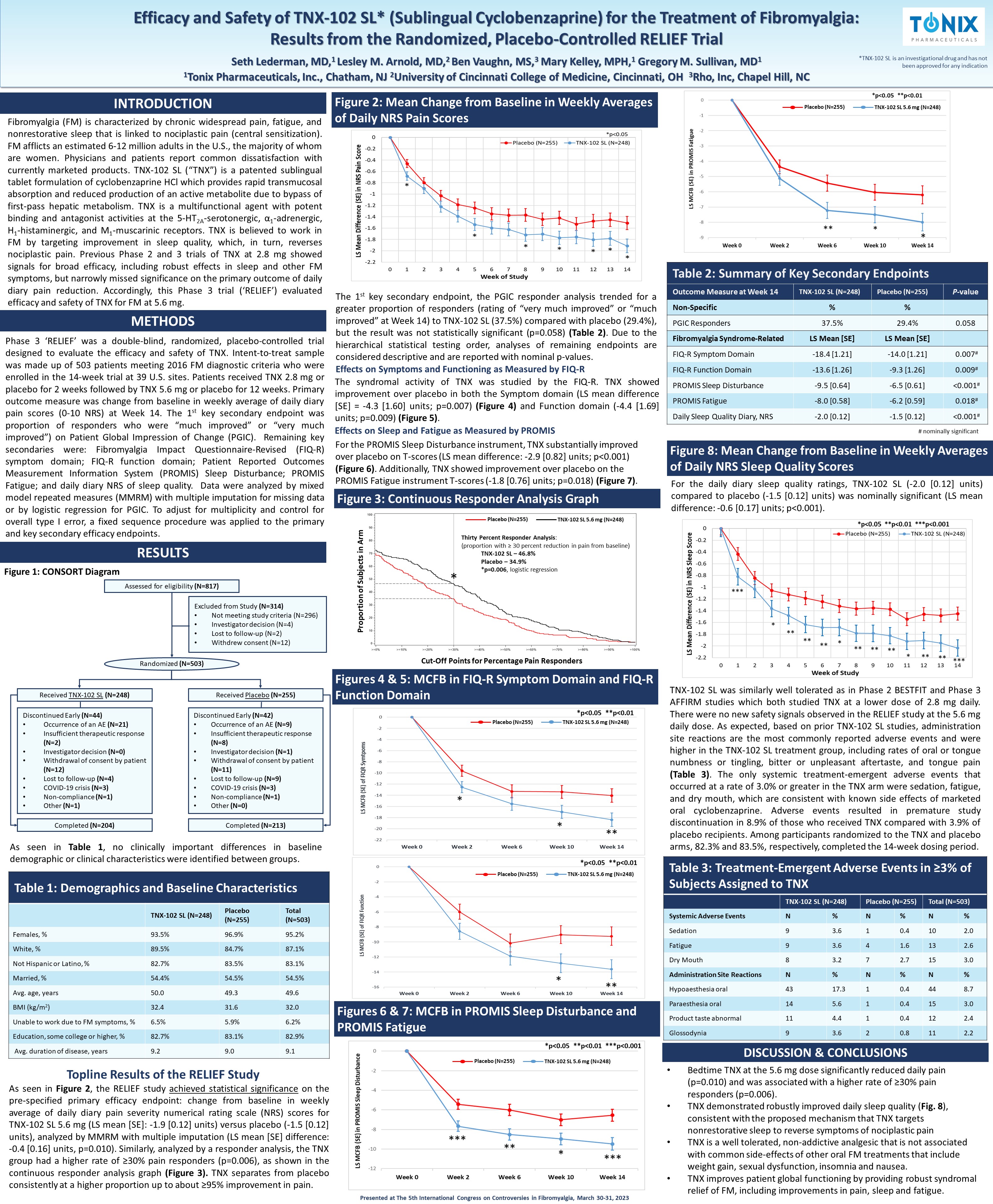
Efficacy and Safety of TNX - 102 SL* (Sublingual Cyclobenzaprine) for the Treatment of Fibromyalgia: Results from the Randomized, Placebo - Controlled RELIEF Trial Seth Lederman, MD, 1 Lesley M. Arnold, MD, 2 Ben Vaughn, MS, 3 Mary Kelley, MPH, 1 Gregory M. Sullivan, MD 1 1 Tonix Pharmaceuticals, Inc., Chatham, NJ 2 University of Cincinnati College of Medicine, Cincinnati, OH 3 Rho, Inc, Chapel Hill, NC *TNX - 102 SL is an investigational drug and has not been approved for any indication INTRODUCTION RESULTS METHODS Fibromyalgia (FM) is characterized by chronic widespread pain, fatigue, and nonrestorative sleep that is linked to nociplastic pain (central sensitization) . FM afflicts an estimated 6 - 12 million adults in the U . S . , the majority of whom are women . Physicians and patients report common dissatisfaction with currently marketed products . TNX - 102 SL (“TNX”) is a patented sublingual tablet formulation of cyclobenzaprine HCl which provides rapid transmucosal absorption and reduced production of an active metabolite due to bypass of first - pass hepatic metabolism . TNX is a multifunctional agent with potent binding and antagonist activities at the 5 - HT 2 A - serotonergic, α 1 - adrenergic, H 1 - histaminergic, and M 1 - muscarinic receptors . TNX is believed to work in FM by targeting improvement in sleep quality, which, in turn, reverses nociplastic pain . Previous Phase 2 and 3 trials of TNX at 2 . 8 mg showed signals for broad efficacy, including robust effects in sleep and other FM symptoms, but narrowly missed significance on the primary outcome of daily diary pain reduction . Accordingly, this Phase 3 trial (‘RELIEF’) evaluated efficacy and safety of TNX for FM at 5 . 6 mg . Phase 3 ‘RELIEF’ was a double - blind, randomized, placebo - controlled trial designed to evaluate the efficacy and safety of TNX . Intent - to - treat sample was made up of 503 patients meeting 2016 FM diagnostic criteria who were enrolled in the 14 - week trial at 39 U . S . sites . Patients received TNX 2 . 8 mg or placebo for 2 weeks followed by TNX 5 . 6 mg or placebo for 12 weeks . Primary outcome measure was change from baseline in weekly average of daily diary pain scores ( 0 - 10 NRS) at Week 14 . The 1 st key secondary endpoint was proportion of responders who were “much improved” or “very much improved”) on Patient Global Impression of Change (PGIC) . Remaining key secondaries were : Fibromyalgia Impact Questionnaire - Revised (FIQ - R) symptom domain ; FIQ - R function domain ; Patient Reported Outcomes Measurement Information System (PROMIS) Sleep Disturbance ; PROMIS Fatigue ; and daily diary NRS of sleep quality . Data were analyzed by mixed model repeated measures (MMRM) with multiple imputation for missing data or by logistic regression for PGIC . To adjust for multiplicity and control for overall type I error, a fixed sequence procedure was applied to the primary and key secondary efficacy endpoints . Figure 1: CONSORT Diagram Assessed for eligibility (N=817) Excluded from Study (N=314) • Not meeting study criteria (N=296) • Investigator decision (N=4) • Lost to follow - up (N=2) • Withdrew consent (N=12) Randomized (N=503) Received TNX - 102 SL (N=248) Received Placebo (N=255) Discontinued Early (N=44) • Occurrence of an AE (N=21) • Insufficient therapeutic response (N=2) • Investigator decision (N=0) • Withdrawal of consent by patient (N=12) • Lost to follow - up (N=4) • COVID - 19 crisis (N=3) • Non - compliance (N=1) • Other (N=1) Discontinued Early (N=42) • Occurrence of an AE (N=9) • Insufficient therapeutic response (N=8) • Investigator decision (N=1) • Withdrawal of consent by patient (N=11) • Lost to follow - up (N=9) • COVID - 19 crisis (N=3) • Non - compliance (N=1) • Other (N=0) Completed (N=204) Completed (N=213) Figures 4 & 5: MCFB in FIQ - R Symptom Domain and FIQ - R Function Domain Figures 6 & 7: MCFB in PROMIS Sleep Disturbance and PROMIS Fatigue Figure 3: Continuous Responder Analysis Graph Table 2: Summary of Key Secondary Endpoints P - value Placebo (N=255) TNX - 102 SL (N=248) Outcome Measure at Week 14 % % Non - Specific 0.058 29.4% 37.5% PGIC Responders LS Mean [SE] LS Mean [SE] Fibromyalgia Syndrome - Related 0.007 # - 14.0 [1.21] - 18.4 [1.21] FIQ - R Symptom Domain 0.009 # - 9.3 [1.26] - 13.6 [1.26] FIQ - R Function Domain <0.001 # - 6.5 [0.61] - 9.5 [0.64] PROMIS Sleep Disturbance 0.018 # - 6.2 [0.59] - 8.0 [0.58] PROMIS Fatigue <0.001 # - 1.5 [0.12] - 2.0 [0.12] Daily Sleep Quality Diary, NRS Table 1: Demographics and Baseline Characteristics Total (N=503) Placebo (N=255) TNX - 102 SL (N=248) 95.2% 96.9% 93.5% Females, % 87.1% 84.7% 89.5% White, % 83.1% 83.5% 82.7% Not Hispanic or Latino, % 54.5% 54.5% 54.4% Married, % 49.6 49.3 50.0 Avg. age, years 32.0 31.6 32.4 BMI (kg/m 2 ) 6.2% 5.9% 6.5% Unable to work due to FM symptoms, % 82.9% 83.1% 82.7% Education, some college or higher, % 9.1 9.0 9.2 Avg. duration of disease, years As seen in Table 1 , no clinically important differences in baseline demographic or clinical characteristics were identified between groups . As seen in Figure 2 , the RELIEF study achieved statistical significance on the pre - specified primary efficacy endpoint : change from baseline in weekly average of daily diary pain severity numerical rating scale (NRS) scores for TNX - 102 SL 5 . 6 mg (LS mean [SE] : - 1 . 9 [ 0 . 12 ] units) versus placebo ( - 1 . 5 [ 0 . 12 ] units), analyzed by MMRM with multiple imputation (LS mean [SE] difference : - 0 . 4 [ 0 . 16 ] units, p= 0 . 010 ) . Similarly, analyzed by a responder analysis, the TNX group had a higher rate of ≥ 30 % pain responders (p= 0 . 006 ), as shown in the continuous responder analysis graph (Figure 3 ) . TNX separates from placebo consistently at a higher proportion up to about ≥ 95 % improvement in pain . Figure 2: Mean Change from Baseline in Weekly Averages of Daily NRS Pain Scores Cut - Off Points for Percentage Pain Responders Proportion of Subjects in Arm * The 1 st key secondary endpoint, the PGIC responder analysis trended for a greater proportion of responders (rating of “very much improved” or “much improved” at Week 14 ) to TNX - 102 SL ( 37 . 5 % ) compared with placebo ( 29 . 4 % ), but the result was not statistically significant (p= 0 . 058 ) (Table 2 ) . Due to the hierarchical statistical testing order, analyses of remaining endpoints are considered descriptive and are reported with nominal p - values . For the PROMIS Sleep Disturbance instrument, TNX substantially improved over placebo on T - scores (LS mean difference: - 2.9 [0.82] units; p<0.001) (Figure 6) . Additionally, TNX showed improvement over placebo on the PROMIS Fatigue instrument T - scores ( - 1.8 [0.76] units; p=0.018) (Figure 7) . The syndromal activity of TNX was studied by the FIQ - R . TNX showed improvement over placebo in both the Symptom domain (LS mean difference [SE] = - 4 . 3 [ 1 . 60 ] units ; p= 0 . 007 ) (Figure 4 ) and Function domain ( - 4 . 4 [ 1 . 69 ] units ; p= 0 . 009 ) (Figure 5 ) . Effects on Sleep and Fatigue as Measured by PROMIS Effects on Symptoms and Functioning as Measured by FIQ - R * * ** *p<0.05 **p<0.01 *p<0.05 **p<0.01 * ** *** ** * *** *p<0.05 **p<0.01 ***p<0.001 Topline Results of the RELIEF Study Figure 8: Mean Change from Baseline in Weekly Averages of Daily NRS Sleep Quality Scores For the daily diary sleep quality ratings, TNX - 102 SL ( - 2 . 0 [ 0 . 12 ] units) compared to placebo ( - 1 . 5 [ 0 . 12 ] units) was nominally significant (LS mean difference : - 0 . 6 [ 0 . 17 ] units ; p< 0 . 001 ) . TNX - 102 SL was similarly well tolerated as in Phase 2 BESTFIT and Phase 3 AFFIRM studies which both studied TNX at a lower dose of 2 . 8 mg daily . There were no new safety signals observed in the RELIEF study at the 5 . 6 mg daily dose . As expected, based on prior TNX - 102 SL studies, administration site reactions are the most commonly reported adverse events and were higher in the TNX - 102 SL treatment group, including rates of oral or tongue numbness or tingling, bitter or unpleasant aftertaste, and tongue pain (Table 3 ) . The only systemic treatment - emergent adverse events that occurred at a rate of 3 . 0 % or greater in the TNX arm were sedation, fatigue, and dry mouth, which are consistent with known side effects of marketed oral cyclobenzaprine . Adverse events resulted in premature study discontinuation in 8 . 9 % of those who received TNX compared with 3 . 9 % of placebo recipients . Among participants randomized to the TNX and placebo arms, 82 . 3 % and 83 . 5 % , respectively, completed the 14 - week dosing period . Table 3: Treatment - Emergent Adverse Events in ≥3% of Subjects Assigned to TNX Total (N=503) Placebo (N=255) TNX - 102 SL (N=248) % N % N % N Systemic Adverse Events 2.0 10 0.4 1 3.6 9 Sedation 2.6 13 1.6 4 3.6 9 Fatigue 3.0 15 2.7 7 3.2 8 Dry Mouth % N % N % N Administration Site Reactions 8.7 44 0.4 1 17.3 43 Hypoaesthesia oral 3.0 15 0.4 1 5.6 14 Paraesthesia oral 2.4 12 0.4 1 4.4 11 Product taste abnormal 2.2 11 0.8 2 3.6 9 Glossodynia DISCUSSION & CONCLUSIONS • Bedtime TNX at the 5.6 mg dose significantly reduced daily pain (p=0.010) and was associated with a higher rate of ≥30% pain responders (p=0.006). • TNX demonstrated robustly improved daily sleep quality ( Fig. 8 ), consistent with the proposed mechanism that TNX targets nonrestorative sleep to reverse symptoms of nociplastic pain • TNX is a well tolerated, non - addictive analgesic that is not associated with common side - effects of other oral FM treatments that include weight gain, sexual dysfunction, insomnia and nausea. • TNX improves patient global functioning by providing robust syndromal relief of FM, including improvements in pain, sleep and fatigue. Presented at The 5th International Congress on Controversies in Fibromyalgia, March 30 - 31, 2023 # nominally significant Thirty Percent Responder Analysis : (proportion with ≥ 30 percent reduction in pain from baseline) TNX - 102 SL – 46.8% Placebo – 34.9% *p=0.006 , logistic regression Placebo (N=255) TNX - 102 SL 5.6 mg (N=248) Placebo (N=255) TNX - 102 SL 5.6 mg (N=248) Placebo (N=255) TNX - 102 SL 5.6 mg (N=248) Placebo (N=255) TNX - 102 SL 5.6 mg (N=248) *p<0.05 **p<0.01 * ** Placebo (N=255) TNX - 102 SL 5.6 mg (N=248) *** * ** ** ** * ** ** ** * ** ** *** *p<0.05 **p<0.01 ***p<0.001