Exhibit 99.01
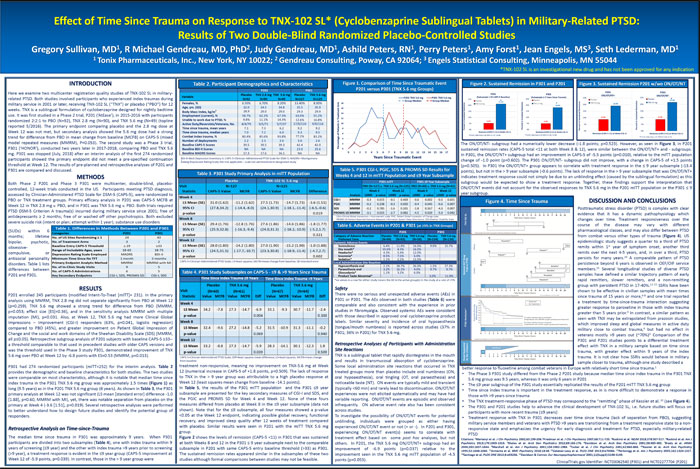
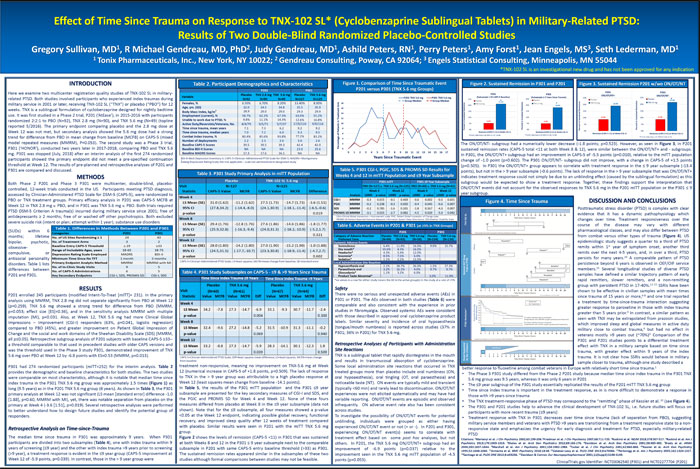
Effect of Time Since Trauma on Response to TNX 102 SL* (Cyclobenzaprine Sublingual Tablets) in Military Related PTSD: Results of Two Double Blind Randomized Placebo Controlled StudiesGregory Sullivan, MD , R Michael Gendreau, MD, PhD , Judy Gendreau, MD , Ashild Peters, RN , Perry Peters , Amy Forst , Jean Engels, MS , Seth Lederman, MD(1)Tonix Pharmaceuticals, Inc., New York, NY 10022; Gendreau Consulting, Poway, CA 92064; Engels Statistical Consulting, Minneapolis, MN 55044*TNX-102 SL is an investigational new drug and has not been approved for any indicationTable 2. Participant Demographics and CharacteristicsThe ON/OT/NT- subgroup had a numerically lower decrease - ( 1.8 points; p=0.523). However, as seen in Figure 3, in P201 sustained remission rates (CAPS-5 total <11 at both Week 8 & 12), were similar between the ON/OT/NT+ and - subgroups. In P301, the ON/OT/NT+ subgroup had an improvement in CAPS-5 of -5.5 points (p=0.010), relative to the mITT population BDI-II=Beck Depression Inventory-II; CAPS-5=Clinician-Administered PTSD Scale for DSM-5; MADRS= Montgomery- change of -1.0 point (p=0.602). The P301 ON/OT/NT- subgroup did not improve, with a change in CAPS-5 of +1.5 points Åsberg Depression Rating Scale; NA=not applicable – scale not administered in designated study (p=0.505). In P301 the ON/OT/NT+ group appears to correlate with treatment response in the = 9 year subsample (-13.4 Table 5. P301 CGI I, PGIC, SDS & PROMIS SD Results for points), but not in the > 9 year subsample (-0.6 points). The lack of response in the > 9 year subsample that was ON/OT/NT+ Table 3. P301 Study Primary Analysis mITT Population Weeks 4 and 12 mITT Population and =9 Year Subsample indicates treatment response could not simply be due to an unblinding effect (caused by the sublingual formulation) as this subgroup would be expected to show a treatment response. Together, these findings support the interpretation that ON/OT/NT events did not account for the observed responses to TNX 5.6 mg in the P201 mITT population or the P301 = 9 year subgroup. DISCUSSION AND CONCLUSIONSPosttraumatic stress disorder (PTSD) is complex with clear evidence that it has a dynamic pathophysiology which CGI-I=Clinical Global Impressions – Improvement scale; PGIC, Patient Global Impression of Change scale; PROMIS SD=Patient-Reported Outcome Measures Information System Sleep Disturbance; SDS=Sheehan Disability Scale changes over time. Treatment responsiveness over the Table 6. Adverse Events in P201 & P301 (at =5% in TNX Groups) course of the disease may vary with different (SUDs) within 6 pharmacological classes, and may also differ between PTSD months; lifetime from combat versus other types of trauma (Figure 4). US bipolar, psychotic, epidemiologic study suggests a quarter to a third of PTSD obsessive- remits within 1(st)year of symptom onset, another third compulsive, or remits over the next 4-5 years, and, in over a third, PTSD antisocial personality persists for many years.(10)A comparable pattern of PTSD disorders. Table 1 lists CAPS-5=Clinician-Administered PTSD Scale; LS=least squares; MCFB=mean change from baseline; SE=standard error persistence beyond 6 years is observed in OEF/OIF service differences between members.(11)Several longitudinal studies of diverse PTSD Table 4. P301 Study Subsamples on CAPS =9 & >9 Years Since Trauma samples have defined a similar trajectory pattern of early P201 and P301. *no values in a row for either study means the AE in the active group(s) in the study at a rate of <5% rapid remitters, slower remitters, and a non-remitting group with persistent PTSD in 17-40%.(12-15)SSRIs have been RESULTS Safety shown to be effective in civilian samples with mean times P201 enrolled 245 participants (modified Intent-To-Treat [mITT]= 231). In the primary There were no serious and unexpected adverse events (AEs) in since trauma of 15 years or more,(6-8)and one trial reported analysis using MMRM, TNX 2.8 mg did not separate significantly from PBO at Week 12 P301 or P201. The AEs observed in both studies (Table 6) were a treatment by time-since-trauma interaction suggesting (p=0.259). TNX 5.6 mg showed a strong trend for difference from PBO (MMRM, comparable and also consistent with the experience in prior greater response to paroxetine in those with index trauma p=0.053; effect size [ES]=0.36), and in the sensitivity analysis MMRM with multiple studies in fibromyalgia. Observed systemic AEs were consistent greater than 5 years prior.(9)In contrast, a similar pattern as imputation (MI), p=0.031. Also, at Week 12, TNX 5.6 mg had more Clinical Global with those described in approved oral cyclobenzaprine product seen with TNX may be extrapolated from prazosin studies, Impressions – Improvement (CGI-I) responders (63%, p=0.041, logistic regression) labels. Similar severity and incidence of oral hypoaesthesia which improved sleep and global measures in active duty compared to PBO (45%), and greater improvement on Patient Global Impression of (tongue/mouth numbness) is reported across studies (37% in military close to combat trauma,(4)but had no effect in Change and the social and work domains of the Sheehan Disability Scale (SDS) (MMRM, P301; 36% in P201) for TNX 5.6 mg. veterans mostly >9 years out (~70%)(3)Comparison of the all p=0.05). Retrospective subgroup analysis of P201 subjects with baseline CAPS-5 =33-- P301 and P201 studies points to a differential treatment a threshold comparable to that used in precedent studies with older CAPS versions and Retrospective Analyses of Participants with Administration effect with TNX in a military sample based on time since was the threshold used in the Phase 3 study P301, demonstrated improvement of TNX Site Reactions trauma, with greater effect within 9 years of the index 5.6 mg over PBO at Week 12 by -6.8 points with ES=0.53 (MMRM, p=0.013). TNX is a sublingual tablet that rapidly disintegrates in the mouth CAPS-5=Clinician-Administered PTSD Scale; Diff=least squares mean difference; LS=least squares; MCFB=mean change trauma. It is not clear how SSRIs would behave in military from baseline and results in transmucosal absorption of cyclobenzaprine. sample closer to trauma, although one study described a P301 had 274 randomized participants (mITT=252) for the interim analysis. Table 2 treatment non-responsive, meaning no improvement on TNX-5.6 mg at Week Some local administration site reactions that occurred in TNX better response to fluoxetine among combat veterans in Europe with relatively short time since trauma.(1)provides the demographic and baseline characteristics for both studies. The two studies 12 (numerical increase in CAPS-5 of +1.8 points, p=0.509). The lack of response treated groups more than placebo include oral numbness (ON, • The Phase 3 P301 study differed from the Phase 2 P201 study because median time since index trauma in the P301 TNX were comparable on most characteristics, although it is notable that median time since to TNX in the > 9 year group was attributable to a high placebo response at oral hypoaesthesia), oral tingling (OT, oral paraesthesia) and 5.6 mg group was 9.5 years, whereas it was only 6 years in P201 index trauma in the P301 TNX 5.6 mg group was approximately 1.5 times (Figure 1) as Week 12 (least squares mean change from baseline -14.1 points). noticeable taste (NT). ON events are typically mild and transient • The =9 year subgroup of the P301 study essentially replicated the results of the P201 mITT TNX 5.6 mg group long (9.5 years) as in the P201 TNX 5.6 mg group (6 years). As shown in Table 3, the P301 In Table 5, the results of the P301 mITT population and the P301 =9 year (typically <60 min) and rarely lead to discontinuation. ON/OT/NT • Time since index trauma is important in the treatment response, as in is more difficult to demonstrate a response in primary analysis at Week 12 was not significant (LS mean [standard error] difference -1.0 subsample are presented for the key secondary measures of CGI-I and SDS, and experiences were not elicited systematically and may have had those with >9 years since trauma [1.88], p=0.60, MMRM with MI), yet, there was notable separation from placebo on the the PGIC and PROMIS SD for Week 4 and Week 12. None of these fours variable reporting. ON/OT/NT events are episodic and observed • The TNX treatment-responsive phase of PTSD may correspond to the “remitting” phase of Kessler et al. (10)(see Figure 4). primary at Week 4 - ( 3.6 [1.51], p=0.019). Several retrospective analyses were performed measures differed from placebo at Week 8 in the =9 year subsample (data not infrequently. ON adverse event rate also has been consistent • The P301 and P201 studies help to advance the clinical development of TNX-102 SL, i.e. future studies will focus on to better understand how to design future studies and identify the potential group of shown). Note that for the =9 subsample, all four measures showed a p-value across studies. participants with more recent trauma (=9 years) responders. <0.05 at the Week 12 endpoint, indicating possible global recovery, functional To investigate the possibility of ON/OT/NT events for potential • Treatment response with TNX in P301 decreases over time since trauma (lack of separation from PBO), suggesting recovery, and improved sleep quality after 12 weeks of treatment compared unblinding, individuals were grouped as either having military service members and veterans with PTSD >9 years are transitioning from a treatment responsive state to a non-with placebo. Similar results were seen in P201 with the mITT TNX 5.6 mg experienced ON/OT/NT event or not (+ or -). In P201 and P301, Retrospective Analysis on Time since Trauma responsive state and emphasizes the urgency for early diagnosis and treatment for PTSD, especially military-related group. experiencing ON/OT/NT event(s) seems to correlate with PTSD The median time since trauma in P301 was approximately 9 years. When P301 Figure 2 shows the levels of remission (CAPS-5 <11) in P301 that was sustained treatment effect based on some post hoc analyses, but not Citations: (1)Martenyi et al. J Clin Psychiatry 2002;63:199-206.(2)Friedman et al. J Clin Psychiatry 2007;68:711-720. (3)Raskind et al. NEJM 2018;378:507-517. (4)Raskind et al. Am J participants are divided into two subsamples (Table 4), one with index trauma within 9 at both Weeks 8 and 12 in the P301 =9 year subsample next to the comparable others. In P201, the TNX 5.6 mg ON/OT/NT+ subgroup had an Psychiatry 2013;170:1003-1010. (5)Shalev et al. Arch Gen Psychiatry 2012;69:166-176. (6)Davidson et al. Arch Gen Psychiatry 2001;58:485-492. (7)Brady et al. JAMA years of screening (=9 year) and the other with index trauma >9 years prior to screening subsample in P201 with same CAPS-5 entry baseline threshold (>33) as P301. improvement of -6.9 points (p=0.037) relative to the 2000;283:1837-1844. (8)Marshall et al. Am J Psychiatry 2001;158:1982-1988. (9)Tucker et al. J Clin Psychiatry 2001;62:860-868. (10)Kessler et al. Arch Gen Psychiatry (>9 year), a treatment response is evident in the =9 year group (CAPS-5 improvement at 1995;52:1048-1060. (11)Armenta et al. BMC Psychiatry 2018;18:48. (12)Galatzer-Levy et al. PLOS ONE 2013;8:e70084. (13)Perkonigg et al. Am J Psychiatry 2005;162:1320-1327. The sustained remission rates appeared similar in the subsamples of these two improvement seen in the TNX 5.6 mg mITT population of -4.5 (14)Santiago et al. PLOS ONE 2013;8:e59236. (15)Davidson & Connor. Eur Neuropsychopharmacol 2001;11(Supp3):S148-S149. Week 12 of -5.9 points, p=0.039). In contrast, those in the > 9 year group were studies although formal comparisons between studies may not be feasible. points (p=0.053).